Definition and cause of Spinal disc herniation - Slipped disc
The back or the vertebral column consists of a series of small round bones (vertebras)that are stacked on top of each other. The rear portion of each vertebra consists of a ring-like bone structure. These rings form a channel in which the spinal cord runs. Departing between each of the vertebrae are two spinal nerves one to each side of the body.
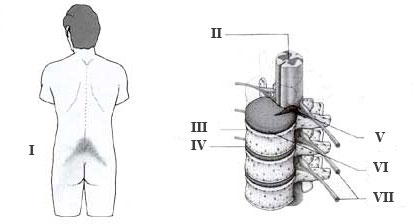
I: Pain location
II: The spinal cord
III: Swirl
IV: Discus
V: Prolapse pressing on nearby nerves
VI: Injured Discus
VII: Nerves
Between vertebras is elastic cartilage slices as a buffer by spinal movements. Each cartilage slice, discs, consists of an outer fixed ring surrounding a core of gel like mass at loads of the spine to the mass of discuses the core is forced out through a weak pointi the surrounding cartilage ring exerting pressure on the neighboring nerve, where it exits the vertebral canal, resulting in pain
Between two adjacent vertebrae lies a discus. A discus is a plate consisting of an outer fibrous ring surrounding and enclosing a central pulpous matter (the nucleus). The discus has primarily a shock absorbing function but does also facilitate movement of the back. The nucleus may break through a weakened outer fibrous ring (a prolapsed disc or spinal herniation) causing the pulpous matter to put pressure directly on the nerve causing direct as well as radiating pain.
The risk of spinal disc herniation increases with age, when the discs are worn thin and thus can not withstand pressure caused by heavy lifting or heavy physical work. Hard physical work with many lifts but also a passive lifestyle without exercise can lead to disc herniation.
The vertebra can be categorized as neck, chest or lumber vertebra. Disc herniation is commonly seen in the lumbar region and to a lesser extend in the neck region. Disc herniation in the thoracic area is very rare. Lumbar disc herniation is typically seen in men of 30-50 years of age.
Symptoms of disc herniation
The symptoms of a prolapse are very different depending on at which level of the spine the herniation is located as well as the level of nerve involvement. The symptoms may appear suddenly for instance in association with a sudden strain of the back or may develop gradually over a long period of time.
The symptoms are:
-
Pain, which is often located to the vertebra at the level of the prolapse, and which may radiate to the arms, neck, back, buttocks or legs. The pain is exacerbated by movement, which puts additional strain on the affected nerve. This is called "sciatic pain".
-
Sensory disturbances located to the neck, arms, back, buttocks or legs.
-
Muscle force reduction and in severe cases spasticity.
-
Reduced nerve reflexes can be observed in both arms and legs.
-
A lumbar herniation may cause incontinence of urine or faeces.
The symptoms can be exacerbated by prolonged sitting or when pressure in the abdomen is increased e.g. during coughing and bowel movement). When the prolapse is only involving one inter vertebral nerve unilateral symptoms are seen, but with larger prolapses, which affect the spinal cord, symptoms can occur in both sides of the body.
Herniation in the neck region will symptoms from the neck and arms, and the neck can be turned into a position that relieves pressure on the inter vertebral nerve. A prolapse involving the lumbar spine may cause symptoms from the legs, buttocks, rectum or bladder.
Prevention and diagnosis
You should avoid any kind of heavy workload especially in awkward positions to the spine. Be that prolonged sedentary work, repetitive heavy lifting or repetitive monotonous twists of the back. If one experiences increasing pain from the back especially in connection with the above movements one should immediately seek medical advice as this may be the early signals of a prolapsing discus.
The doctor may, based on the work history, symptoms and a thorough examination of the back, assess whether there is suspicion of a prolapsed discus. In some cases it will be necessary to perform an MRI scan to determine whether a discus is prolapsed.
Treatment of disc herniation
With the right treatment from a qualified medical specialist most patients will recover from the symptoms of prolapsed discus. It requires however intensive physiotherapeutic training with stretching and muscle training exercises, and it may take a long time.
Herniation in the neck region can benefit from wearing a supportive neck collar for a few weeks. It is important to avoid the physical strain that caused the symptoms, even after the symptoms may have disappeared. Immediate pain and reoccurring pain may be alleviated with regular pain killers.
In cases where there is muscle paralysis, urine- and stool incontinence or the above treatment has not been effective, the herniation may be treated surgically. The aim of surgery is to create more space for the inter-vertebral nerves. Sometimes the surgeon may choose to make the part of the back around the herniation stiff in order to avoid that future movement of the back will lead to renewed herniation.
Prognosis and complications
Most patiens are likely to be symptom-free without surgery. The patient may however need to change job or to reduce working hours to limit the risk of re-herniation. 4 out of 5 will after surgery become symptom free and be able to work again. The last fifth will continue to experience periodic symptoms, and common to all is an increased risk of re-herniation.
The most dreaded complication of a prolapsed discus is permanent damage to the spinal cord.
Læs denne artikel på dansk |